Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124

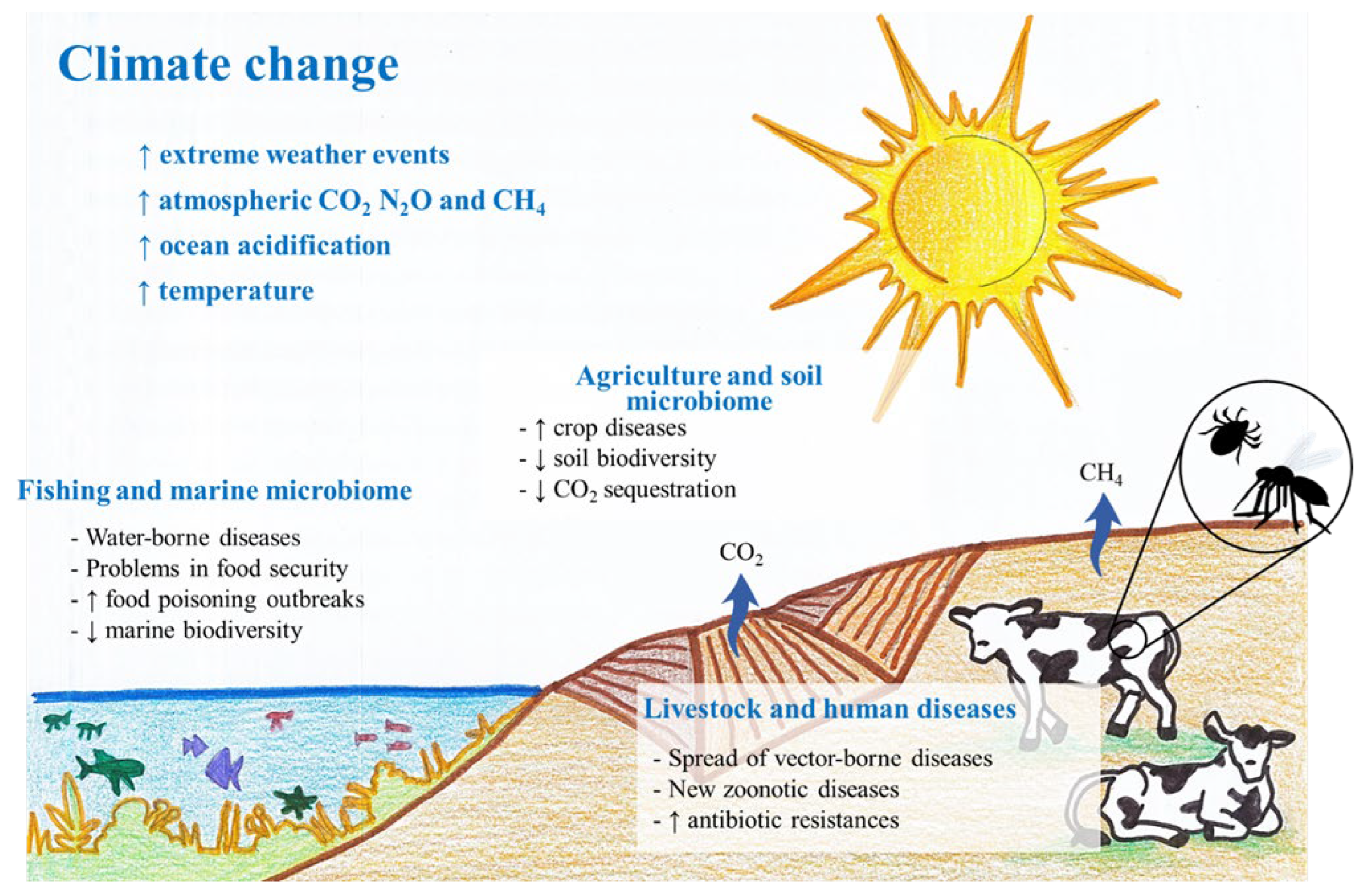
Climate change accelerates the spread of infectious diseases by altering ecosystems and affecting vectors. Changes in temperature and precipitation patterns expand habitats for disease-carrying organisms.
Climate change has emerged as a formidable force influencing global health. By disrupting natural habitats and weather patterns, it creates ideal conditions for vectors such as mosquitoes and ticks to thrive, leading to a rise in diseases like malaria, dengue, and Lyme disease.
These shifts in climate not only extend the geographical reach of these diseases but also impact the timing and intensity of outbreaks. As such, health systems must adapt to manage the increased risk of infections. Understanding the link between climate change and infectious diseases is critical for developing effective public health strategies and mitigating potential crises. Researchers and policymakers alike are calling for urgent action to address the health implications of a warming planet.
The bond between our changing environment and public health paints a complex picture. This intersection, the Climate-Disease Nexus, reveals the direct and indirect effects that a warming planet can have on the spread of infectious diseases. It’s not just hotter days; it’s about understanding how these rising temperatures and erratic weather patterns move the pieces in a global health puzzle.
As thermometers rise, several pathogens find a more favorable breeding ground. With warmth, some germs multiply rapidly. Diseases carried by vectors like mosquitoes and ticks also surge. These carriers thrive and expand their territories in the heat, taking diseases such as malaria and dengue fever to new regions.
Not only does temperature rise, but our weather also turns unpredictable. Sudden and severe weather changes can lead to devastating health outcomes. Heavy rainfalls and flooding can contaminate water supplies, causing outbreaks of cholera and other waterborne diseases. Droughts, equally alarming, reduce available clean water, increasing the risk of diseases.
| Weather Event | Possible Diseases |
|---|---|
| Heavy Rainfall | Cholera, Mosquito-borne diseases |
| Long Dry Spells | Food-borne illnesses, Respiratory issues |
Understanding these connections helps us prepare. Knowing the risks allows for better disease monitoring and prevention. In a warmer world, proactive health measures become increasingly vital. Communities need to adapt and strengthen defenses against these ever-evolving health challenges.

Credit: www.cdc.gov
Climate change is not just about weather. It affects our health too. When the Earth gets warmer, dangerous bugs travel to new places. These bugs can make people sick. We call these bugs “vectors.” Let’s explore how climate change is helping some of these vectors spread diseases further than ever.
Mosquitoes love warm weather. As the planet heats up, mosquitoes move to new areas. They bring diseases with them. An example is malaria. It’s on the rise in places that used to be too cool for mosquitoes. These insects are not just annoying. They can carry deadly diseases.
People must be ready. We need to stop mosquitoes from biting us. We can wear insect repellent. We can also remove standing water where mosquitoes breed.
Ticks are also on the move. Climate change helps ticks survive in colder places. They carry diseases, such as Lyme disease. More ticks in more places mean more chances to get sick. Ticks live in tall grass and wooded areas. They wait for humans or animals to come by. Then they latch on and bite.
| Tick Type | Diseases Transmitted | Newly Affected Areas |
|---|---|---|
| Deer Ticks | Lyme Disease | Northward into Canada |
| Lone Star Ticks | Ehrlichiosis | Midwestern and Eastern USA |
| Wood Ticks | Rocky Mountain Spotted Fever | More states in the USA |
Protecting against tick bites is important. Wear long sleeves and long pants in risky areas. Check yourself for ticks after being outdoors. Keep your yard clear of tall grass and leaves where ticks hide.
The link between climate change and infectious diseases is becoming clearer, especially as we witness changes in disease patterns around the globe. Of significant concern is the rise in water-borne illnesses, often directly correlated with shifts in precipitation patterns. Extreme weather events, including heavy rainfall, can disrupt the delicate balance of ecosystems, affecting human health in ways we are only beginning to understand.
Intense downpours can lead to overflow of sewage systems and floods. These conditions are perfect for bacteria and viruses to proliferate. Dangerous pathogens find their way into our drinking water and food sources, posing severe risks to our health.
Floods, one of the most immediate consequences of heavy rains, create an environment where water-borne diseases thrive. The stagnant waters act like giant petri dishes, allowing organisms to grow and spread rapidly.
| Infection Type | Common Diseases | Transmission Method |
|---|---|---|
| Parasitic | Giardiasis, Cryptosporidiosis | Contaminated water |
| Bacterial | Typhoid Fever, Leptospirosis | Contact with water |
| Viral | Hepatitis E, Norovirus | Consuming tainted water |
These spills of dangerous microorganisms can eventually lead to wide-scale health crises, especially in areas where healthcare systems are already under pressure.
The relentless march of climate change bears upon all aspects of life on Earth, reshaping the environment and influencing the spread and severity of plant and animal diseases. The agricultural sector feels this impact profoundly as pathogens that harm crops and livestock respond to climatic shifts. Understanding these changes is key to ensuring food security and managing risks to our health and the environment.
Temperature and precipitation are critical factors for crop diseases. Warmer climates can lead to the expansion of pests and pathogens into new areas, putting crops at risk. Increased humidity and wet conditions may promote the growth of fungal and bacterial diseases. Conversely, drought can stress plants, making them more vulnerable to infections.
Climate change also influences diseases in livestock, with higher temperatures and altered rainfall patterns stressing animals and altering their susceptibility to diseases. This stress can weaken their immune systems, leading to an increase in infections.
Zoonotic diseases, which are transmitted from animals to humans, pose an even greater risk as changes in habitat and climate bring humans into closer contact with wildlife. Instances of zoonoses, such as bird flu or Lyme disease, could surge as vectors like mosquitoes and ticks expand their geographic range.
| Factor | Effect on Livestock | Effect on Zoonotic Diseases |
|---|---|---|
| Temperature changes | Heat stress, breeding patterns alter | Spread to new areas |
| Altered rainfall | Waterborne illnesses, grazing changes | Changes in disease vectors’ habitats |
| Increased CO2 levels | Plant quality affects nutrition | Vectors thrive, elevating disease risk |
The battle against infectious diseases faces a daunting new challenge. Climate change is not only affecting our environment but also the way diseases spread. A warmer climate means that infectious diseases can thrive in new areas, putting public health systems on high alert. This means that our hospitals, clinics, and health workers are facing unprecedented pressures, having to deal with emerging health threats in an already stressed environment. In this section, we explore the strains on resources and the challenges in responding to new illnesses as a consequence of our changing climate.
Healthcare systems worldwide are finding their resources stretched thin. The increase in climate-sensitive diseases, such as malaria and dengue fever, is leading to a surge in demand for medical attention, medicines, and public health interventions. This can overwhelm existing infrastructure and limit the ability of healthcare providers to respond to patients’ needs effectively. Resource allocation becomes a critical concern, with vital supplies and personnel often in short supply.
Adapting to the new reality of climate-related health risks means preparing for diseases that may not have been previously encountered in certain regions. It is crucial that global health systems develop strategies to identify, monitor, and combat these new threats. Preparing for climate-linked diseases requires not only research into emerging pathogens but also building robust healthcare infrastructures that can withstand the challenges posed by a changing environment.
| Preparation Aspect | Action Required |
|---|---|
| Disease Surveillance | Improve detection and reporting systems. |
| Healthcare Infrastructure | Develop resilient facilities and networks. |
| Medical Research | Focus on vaccines and treatments for emerging diseases. |
| Public Education | Spread awareness about prevention and symptoms. |
Collaboration across borders is also essential to strengthen global response against climate-induced health risks. A cohesive effort amongst nations helps to share knowledge, resources, and best practices, making it possible to mount an effective response to new and existing infectious diseases accelerated by climate change.

Credit: www.news-medical.net
Climate change poses a real threat to public health, notably by influencing the patterns of infectious diseases. The success of efforts to combat these rising health risks hinges on two critical approaches: mitigation and adaptation. Mitigation involves reducing the causes of climate change, while adaptation strategies aim to minimize the health impacts by improving resilience. The connection between climate change and infectious diseases calls for a proactive stance in both realms.
Effective disease surveillance systems are vital in detecting outbreaks early. Quick action can limit spread. By collecting climate-related data, we can predict disease hotspots. Community health workers need training to recognize climate-sensitive diseases. This way, early warning systems become robust.
Technology plays a key role here. Through mobile apps and online platforms, real-time data sharing becomes possible. Advanced analytics can then pinpoint potential outbreaks. Investment in research aids in understanding the link between climate variables and disease patterns.
International collaboration also proves critical. Shared global databases enhance disease tracking capabilities. This strengthens overall infection control frameworks. Countries can thus coordinate efforts against common threats.
Integrating climate action with disease prevention requires a holistic view. It involves considering health needs in climate-related projects. For instance, when building flood defenses, one must think about vector breeding sites.
Infrastructure development should incorporate disease prevention measures. Green spaces in urban areas can diminish heat impacts and control disease vectors. Smart urban planning can thus reduce climate change effects and disease spread.
Public health policies must reflect this dual approach. Vaccination campaigns can align with climate resilience activities. Public education on disease prevention should also include climate change impacts. By doing so, communities become more informed and resilient.
At every step, health professionals and climate scientists must collaborate. They need to share insights to devise effective strategies. Cross-sector partnerships bring together different expertise. This can result in groundbreaking solutions for both climate change and infectious diseases.
Credit: www.mdpi.com
Climate change can alter transmission patterns of infectious diseases. Warmer temperatures may expand the habitats of disease-carrying vectors, like mosquitoes, leading to a wider spread of diseases such as malaria and dengue. It also affects the timing and intensity of disease outbreaks.
Yes, climate change can increase pandemic risks. It can disrupt natural ecosystems, forcing wildlife to migrate and possibly come into closer contact with humans. This change may facilitate the jump of new pathogens from animals to humans, potentially leading to pandemics.
Certain weather conditions can foster environments conducive to pathogens. For instance, increased humidity or rainfall might boost mosquito breeding rates, raising the risk of vector-borne diseases. Conversely, drought can concentrate pathogens in shrinking water supplies, leading to waterborne disease spikes.
Yes, regions with less infrastructure or healthcare resources are more vulnerable to climate-induced disease risks. Places with warmer climates, like tropical areas, may face an increased burden from vector-borne illnesses. Low-lying islands and coastal regions are also at risk for waterborne diseases after extreme weather events.
As we navigate the complexities of global health, the link between climate change and infectious diseases is unequivocal. Vigilance and adaptation are imperative in our ongoing battle against these evolving threats. Preventative measures and global cooperation will be the keystone for ensuring a healthier planet and populace.
By understanding this connection, we wield the power to enact change and safeguard our future.

