Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124

Behavioral interventions for frontotemporal dementia include structured routines and environmental modifications. Personalized therapeutic activities and caregiver education are also key.
Frontotemporal dementia (FTD) is a challenging neurological condition affecting personality, behavior, and language. Early diagnosis plays a pivotal role in managing FTD effectively. Care strategies focus on creating a supportive environment that caters to individual needs. Structured daily routines help stabilize behaviors, while simplifying tasks enables people with FTD to maintain a level of independence.
Therapeutic activities tailored to the patient’s interests can provide meaningful engagement and improve quality of life. Educating caregivers is crucial as it equips them with strategies to handle difficult behaviors and fosters a deeper understanding of the condition. Successful management of FTD requires a multidisciplinary approach including neurologists, psychiatrists, and occupational therapists to adapt interventions as the disease progresses.
Credit: www.mdpi.com
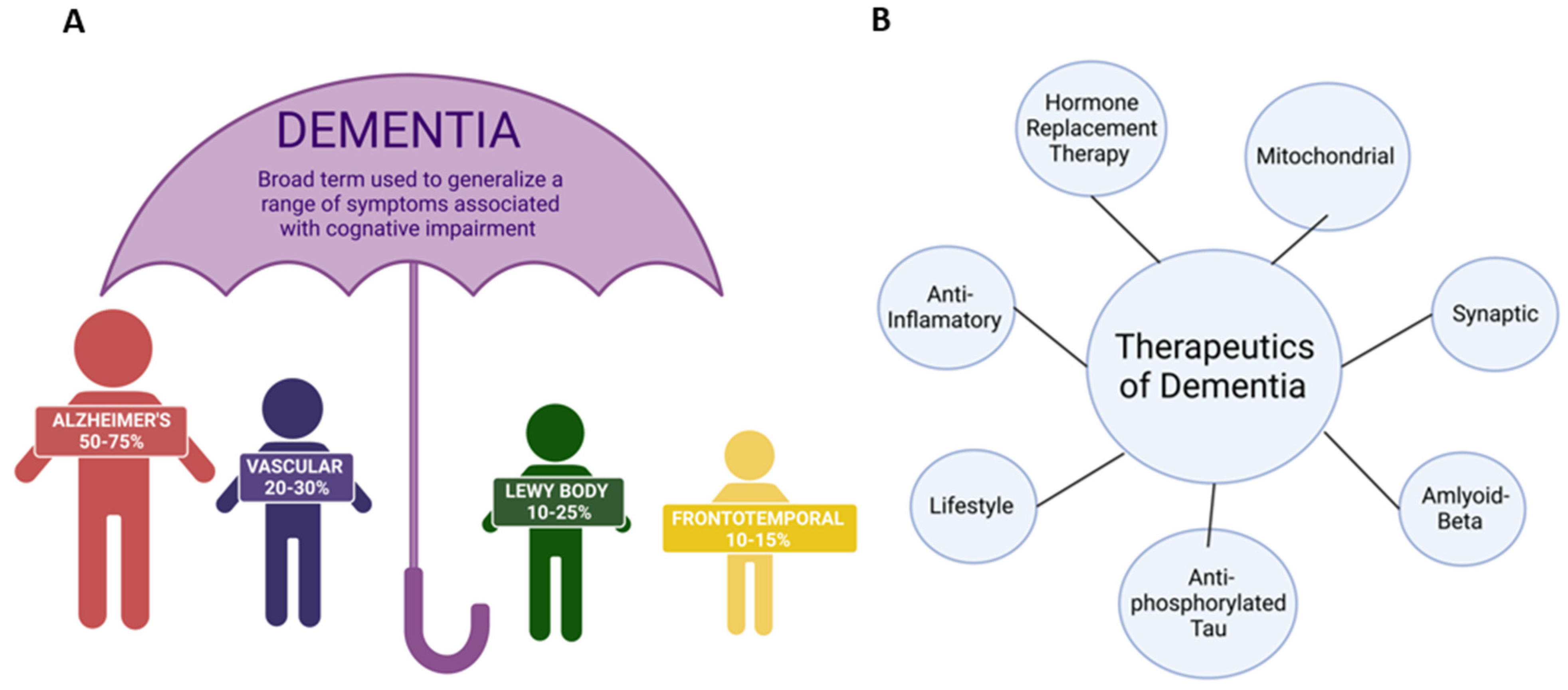
Frontotemporal Dementia, known as FTD, poses unique challenges. Unlike other forms of dementia, FTD often strikes at a younger age. It affects personality and behavior profoundly. This section dives deep into the complexities of FTD. The focus here is on understanding FTD’s nuances. This leads to better management and care strategies for those affected.
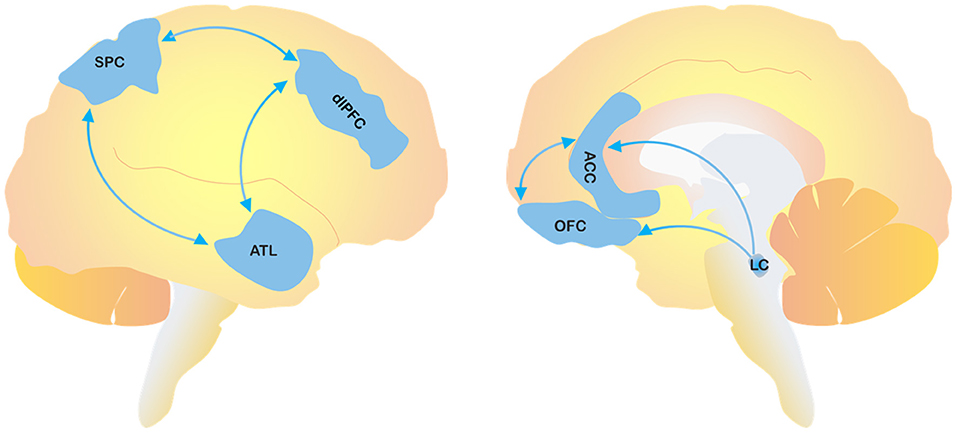
Frontotemporal Dementia (FTD) is a group of brain disorders. It affects the frontal and temporal lobes. These areas control decision-making, behavior, emotion, and language.
FTD presents in varied ways. Some common symptoms include:
| Behavioral Variant FTD (bvFTD) | Primary Progressive Aphasia (PPA) |
|---|---|
| Impulsivity and apathy | Speech and language difficulties |
| Socially inappropriate behavior | Slow, effortful speech |
| Lack of empathy | Difficulty understanding words |
FTD’s impact is profound. It can turn a patient’s world upside down. Family members may notice:

Credit: www.sciencedirect.com
Behavioral Management in Frontotemporal Dementia (FTD) serves as a vital role in caring for patients experiencing the unique challenges of this condition. By adopting tailored strategies, caregivers can effectively navigate the behavioral changes in FTD. Let’s discuss these essential interventions.
Understanding and managing the behavioral symptoms of FTD starts with establishing some core principles:
Effective communication can alleviate many issues that arise with FTD:
A calming and supportive environment is crucial for FTD patients:
Caregivers need tools and strategies to maintain their well-being:
Frontotemporal Dementia (FTD) presents unique challenges for caregivers and health professionals. Strategies addressing behavioral changes can significantly improve the quality of life for both patients and their families. Proven interventions often blend non-pharmacological and, when necessary, pharmacological approaches. Each strategy plays a critical role in managing the complex behavioral symptoms of FTD.
Non-pharmacological interventions offer first-line strategies to modify behaviors without medications. Simple adjustments in the home environment and communication techniques can lead to remarkable benefits.
A structured daily routine brings predictability, reducing stress for individuals with FTD. Incorporating enjoyable and therapeutic activities fosters a sense of purpose.
| Time of Day | Activity |
|---|---|
| Morning | Gentle exercise |
| Afternoon | Art or music therapy |
| Evening | Relaxation techniques |
Engaging the senses can soothe and reduce problematic behaviors. Tailored to individual preferences, sensory experiences include touch, sound, smell, and sight.
Technology assists in managing FTD behaviors. Apps and devices assist with memory, routine, and provide stimulation. They also offer caregiver support through monitoring and reminders.
Pharmacological intervention becomes an option when behaviors pose a risk or significantly interfere with daily life. Consultation with a specialist is essential before starting any medications.
Credit: www.frontiersin.org
Implementing behavioral interventions for Frontotemporal Dementia (FTD) presents unique hurdles. Each person with FTD experiences symptoms differently. This demands tailored approaches for care. Constantly adapting strategies is vital to match the progressive nature of the disease. Moreover, ethical considerations must take center stage to ensure respect and dignity for patients. Determining the success of these interventions hinges on enhancing the quality of life for those affected.
FTD affects everyone differently. Tailoring behavioral interventions to individual symptoms, preferences, and abilities is crucial. This personalization leads to more effective management of challenging behaviors.
Some keys to understanding these needs include:
As FTD progresses, symptoms evolve and intensify. Behavioral strategies must adapt accordingly. Staying one step ahead requires:
Ethical care is paramount in behavioral interventions. Respecting the patient’s autonomy while ensuring safety can be challenging. Ethical considerations should include:
| Consideration | Details |
|---|---|
| Informed Consent | Ensuring the patient or legal guardian understands the intervention |
| Dignity | Upholding the patient’s dignity at all times |
| Non-maleficence | Avoiding harm to the patient through interventions |
Succcess in behavioral interventions is not just about reducing symptoms. It is about improving quality of life. Measures include:
Regular surveys and check-ins with patients and caregivers help track this progress.
The Future of FTD Behavioral Interventions holds much promise as we continue to explore new ways to support those affected by Frontotemporal Dementia (FTD). Innovative research, emerging therapies, enhanced caregiver training, and technology promise to improve quality of life for patients and families alike. Let’s dive into the potential developments on the horizon.
Cutting-edge studies are continuously unveiling new insights into FTD. Emerging treatments focus on neuroplasticity and the brain’s ability to reform connections. Future therapies may include medications that target specific brain cells or pathways implicated in FTD.
Caregiver empowerment is a cornerstone in managing FTD. Training programs are evolving, teaching caregivers behavioral management skills and self-care techniques. Support groups provide a platform for sharing experiences and advice, reducing caregiver burnout and facilitating better patient care.
Technology stands to revolutionize FTD care. From apps that assist with daily tasks to AI-driven diagnostic tools, technological advancements can offer significant support. Developments in telemedicine allow for remote consultations, making specialist care more accessible.
Collaboration between specialists is key to exceptional FTD care. An interdisciplinary approach brings together neurologists, psychologists, speech therapists, and more, ensuring a comprehensive care plan. Interdisciplinary care models are paving the way for coordinated, personalized treatment strategies.
Treating frontotemporal dementia (FTD) behavior involves medication like antidepressants, behavioral interventions, and structured daily routines. Support groups and therapy can help caregivers.
Frontotemporal dementia (FTD) causes various behavioral changes, including impulsivity, apathy, social withdrawal, and loss of empathy. Personality modifications and inappropriate social behavior are also common. These changes impact relationships and daily activities significantly.
Management strategies for frontotemporal dementia include medication to alleviate symptoms, targeted therapies, and supportive care. Engaging in speech and occupational therapy can improve communication and daily function. Support groups and counseling benefit both patients and caregivers.
Agitation in FTD is often managed with non-drug strategies, such as environmental modifications and therapeutic activities. If necessary, physicians may prescribe medication to alleviate symptoms, prioritizing safety and minimal side effects. Consulting a healthcare professional is crucial for personalized treatment plans.
Navigating the landscape of frontotemporal dementia requires compassion and knowledge. Effective behavioral interventions can profoundly impact patients’ quality of life. By staying informed and empathetic, caregivers can tailor support to each unique situation. The journey isn’t simple, but with the right strategies, it’s possible to manage symptoms and foster positive environments for those affected.
Embrace the challenge and make a meaningful difference.