Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Functional movement assessment in physical therapy evaluates mobility, stability, and strength to identify movement dysfunctions and prevent injuries. By analyzing how individuals move, therapists can create personalized treatment plans to improve function and performance.
The assessment involves observing and testing various functional movements to pinpoint limitations and asymmetries, guiding targeted interventions for optimal outcomes. Assessing functional movement not only aids in injury prevention but also enhances overall physical health and quality of life. Therapists use the information gathered from these assessments to address movement patterns and restore functional mobility for their patients.
Through precise assessment and tailored interventions, physical therapists help individuals move better and live healthier lives.
Functional Movement Assessment plays a crucial role in Physical Therapy as it allows therapists to identify underlying movement dysfunctions. By evaluating how individuals move during daily activities, therapists gain valuable insights into their musculoskeletal health and overall functionality.
Assessing how individuals perform fundamental movements helps pinpoint any deviations or imbalances that may lead to injuries or impact their quality of life. Through precise evaluation, therapists can detect asymmetries, weaknesses, or compensations that affect the body’s ability to move efficiently.
By addressing movement dysfunctions early on, therapists can develop targeted interventions to improve movement patterns and enhance functional capabilities. This proactive approach helps individuals operate safely in their daily activities and reduces the risk of future injuries.

Credit: www.udemy.com
Key Components of Functional Movement Assessment:
Assessing range of motion at each joint is critical for identifying restrictions in movement.
Evaluating the strength of muscles helps in understanding imbalances and weaknesses.
Observing the alignment of the body can reveal compensations and deviations from proper posture.
When it comes to physical therapy, conducting an accurate assessment of a patient’s functional movement is crucial for developing an effective treatment plan. Physical therapists utilize various tools and techniques to evaluate a patient’s functional movement, helping to identify strengths, weaknesses, and areas for improvement.
Gait analysis is a fundamental component of functional movement assessment in physical therapy. It involves the observation of an individual’s walking pattern, including their stride length, step width, and overall gait mechanics. By analyzing a patient’s gait, physical therapists can identify abnormalities or asymmetries that may be contributing to their functional limitations.
Manual muscle testing is another essential tool used in physical therapy assessments. This technique involves the application of resistance to specific muscles to determine their strength and function. By systematically testing various muscle groups, physical therapists can pinpoint areas of weakness or imbalance, guiding the development of targeted interventions.
Functional movement assessment is an essential tool that physical therapists use to evaluate a patient’s movement patterns, identify limitations, and design personalized treatment plans. By integrating functional movement assessment into their practice, therapists can accurately pinpoint the root cause of musculoskeletal issues and address them with targeted therapies. This approach focuses on improving overall movement quality, eliminating pain, and enhancing functional abilities for a healthier and more active lifestyle.
With functional movement assessment as a cornerstone of their practice, physical therapists can customize treatment plans to address each patient’s unique needs. By analyzing movements such as squatting, lunging, and reaching, therapists gain valuable insights into any existing imbalances, asymmetries, or dysfunctions in the patient’s musculoskeletal system. Armed with this information, therapists can develop tailored treatment plans that target those specific problem areas, promoting optimal movement patterns and preventing future injuries.
Integrating functional movement assessment into physical therapy practice also helps therapists measure a patient’s progress accurately. Regular reassessment allows therapists to gauge improvements in movement quality, strength, and mobility over time. By re-evaluating movement patterns at various stages of the treatment process, therapists can identify areas where the patient has made significant progress and areas demanding more attention. This ensures that therapy sessions remain focused, goal-oriented, and effective in achieving the desired outcomes.
Functional movement assessment plays a crucial role in physical therapy. By evaluating how well patients move, therapists can identify areas of dysfunction and develop targeted treatment plans. However, there are certain challenges and considerations that need to be taken into account when using functional movement assessment. This article will explore two important factors that influence the effectiveness of this assessment: complex cases and patient cooperation.
Functional movement assessment can be particularly challenging when dealing with complex cases, such as patients with multiple musculoskeletal or neurological conditions. These cases often involve intricate movement patterns and require a comprehensive understanding of underlying pathologies. Therapists must carefully analyze and interpret the gathered data to accurately assess the patient’s functional limitations.
In complex cases, it may be beneficial to use a combination of subjective and objective measures, including patient history, physical examination, and diagnostic tests. This multifaceted approach allows therapists to gain a comprehensive picture of the patient’s condition and better tailor interventions to their specific needs. Additionally, collaborating with other healthcare professionals, such as orthopedic surgeons or neurologists, can provide valuable insights and enhance the accuracy of the functional movement assessment in complex cases.
Patient cooperation is another crucial consideration in functional movement assessment. It is essential that patients actively engage in the assessment process and follow instructions to ensure accurate data collection. Lack of cooperation can lead to unreliable results and undermine the overall effectiveness of the assessment.
To enhance patient cooperation, therapists should establish clear communication and rapport with their patients. They need to explain the purpose of the assessment and its relevance to the treatment plan. By educating patients about the importance of their active participation, therapists can motivate them to exert their best effort during the assessment.
The 7 basic functional movement tests are squat, hinge, push, pull, lunge, rotate, and walk. These tests assess fundamental movement patterns for strength and mobility. Regularly performing these tests can improve overall fitness and prevent injury.
A functional movement assessment evaluates how well the body moves during activities to identify imbalances and limitations that may lead to injury.
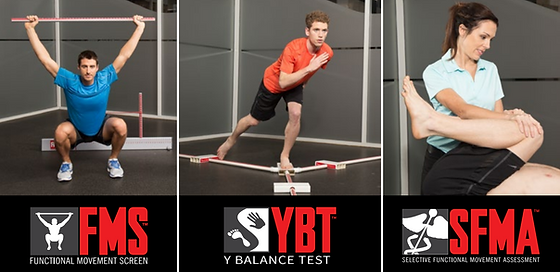
FMS in physical therapy stands for Functional Movement Screen, a system to evaluate and improve movement patterns.
Functional mobility assessment evaluates an individual’s ability to move and perform daily activities. It helps identify limitations and develop tailored intervention plans. This assessment is crucial for understanding patients’ capabilities and enhancing their overall quality of life.
Functional movement assessment plays a crucial role in physical therapy, aiding practitioners in identifying movement dysfunctions and creating tailored treatment plans. By honing in on the body’s mechanics, therapists can address underlying issues and promote long-term recovery and performance. Embracing this holistic approach can lead to improved patient outcomes and overall well-being.

