Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
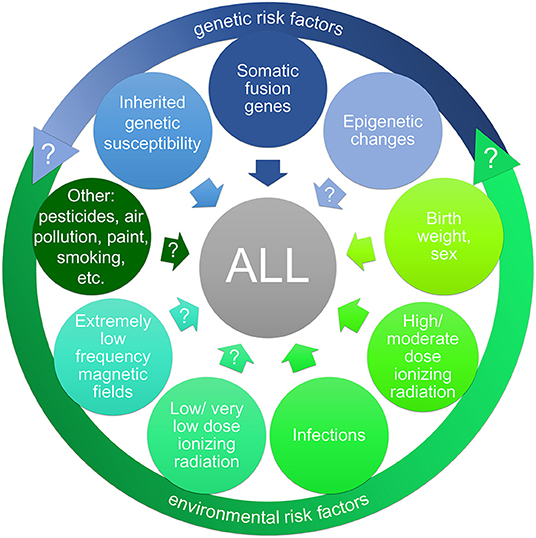
Genetic factors play a crucial role in the risk of developing leukemia, a comprehensive overview indicates. In the following explanation, we will delve into various genetic elements that contribute to the likelihood of developing this type of cancer.
Additionally, we will explore how these factors interact with environmental influences to shape an individual’s susceptibility to leukemia. By understanding the genetic components involved, we can gain insights into potential preventive measures and targeted treatment strategies. This article aims to provide a concise yet comprehensive overview of the role of genetic factors in leukemia development.
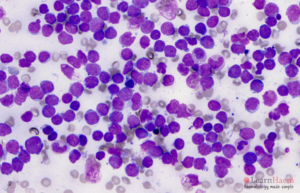
Leukemia is a type of cancer that affects the blood and bone marrow, resulting in an abnormal production of white blood cells. It is a complex condition influenced by a combination of environmental and genetic factors. While environmental factors like exposure to radiation or certain chemicals contribute to the risk of developing leukemia, the role of genetic factors cannot be overlooked. One of the key genetic factors involved in leukemia is chromosomal abnormalities. These abnormalities can occur spontaneously or be inherited from a parent. Certain genetic mutations, such as alterations in genes responsible for controlling cell growth and division, can increase the risk of leukemia. Additionally, variations in genes involved in DNA repair mechanisms or immune system function can also impact an individual’s susceptibility to the disease. Family history is another important genetic factor to consider. Individuals with a close relative who has had leukemia are at a higher risk of developing the disease themselves. This suggests a genetic predisposition to leukemia, although specific genes or mutations responsible for this familial association are still being researched. Furthermore, genetic factors may influence how individuals respond to leukemia treatments. Variations in genes involved in drug metabolism or drug targets can affect the effectiveness and potential side effects of certain therapies. Understanding an individual’s genetic makeup can help personalize treatment approaches and improve outcomes. Genetic factors are integral to the risk of developing leukemia. By studying and recognizing these genetic elements, we can gain a deeper understanding of the disease and develop targeted strategies for prevention, early detection, and treatment. Healthcare providers and researchers continue to explore the intricacies of genetic factors in leukemia to improve patient care and outcomes.

Leukemia, a type of cancer that affects the blood and bone marrow, is a complex disease with various contributing factors. While environmental factors and lifestyle choices play a role in the development of leukemia, genetic factors also significantly impact an individual’s risk. In this section, we will explore the role of genetics in leukemia and delve into the different types of genetic mutations associated with this disease.
Genetics is an essential component in understanding the development of leukemia. Certain genetic mutations or alterations can disrupt the normal functioning of cells, leading to the uncontrolled growth of abnormal cells in the bone marrow and blood. These mutations can be inherited from parents or acquired during a person’s lifetime.
When it comes to inherited genetic factors, individuals with a family history of leukemia are at a higher risk of developing the disease. Research has shown that certain genetic changes, such as chromosomal abnormalities or gene mutations, can be passed down from generation to generation, increasing the likelihood of leukemia occurrence within the family.
Additionally, acquired genetic mutations, known as somatic mutations, can develop in a person’s cells over time due to various factors like exposure to radiation, chemicals, or certain viral infections. These mutations alter the DNA sequence, affecting the regulation of cell growth and division, ultimately contributing to the development of leukemia.
In leukemia, different types of genetic mutations have been identified, each associated with specific subtypes of the disease. Here are some of the most common types:
| Type of Genetic Mutation | Associated Subtypes of Leukemia |
|---|---|
| Chromosomal translocations | Acute lymphoblastic leukemia (ALL), acute myeloid leukemia (AML) |
| Gene amplifications | Chronic myeloid leukemia (CML) |
| Point mutations | Acute myeloid leukemia (AML), chronic lymphocytic leukemia (CLL) |
These genetic mutations can cause disruptions in critical cellular processes, including cell growth, division, and apoptosis, leading to the abnormal formation of blood cells and the onset of leukemia.
Understanding the role of genetic factors and the different types of genetic mutations associated with leukemia is crucial for early detection, targeted therapies, and personalized treatment approaches. By unraveling the intricate relationship between genetics and leukemia, researchers strive to improve patient outcomes and pave the way towards more effective interventions in the future.
Inherited genetic factors play a crucial role in determining an individual’s risk of developing leukemia, a type of blood cancer. Understanding these genetic risk factors can help identify individuals who may be at a higher risk and enable early detection and intervention strategies. In this section, we will delve into two significant aspects of inherited genetic risk: family history and leukemia, as well as genetic syndromes associated with leukemia.
Having a family history of leukemia can increase an individual’s risk of developing the disease. If a close family member, such as a parent or sibling, has been diagnosed with leukemia, the likelihood of developing the disease is higher. Genetic mutations or abnormalities that can be passed down from one generation to another may contribute to this increased risk. It is important for individuals with a family history of leukemia to be proactive in their healthcare, undergoing regular check-ups and screenings to detect any potential signs or symptoms of the disease.
Certain genetic syndromes have been identified as being associated with an elevated risk of developing leukemia. These syndromes are characterized by specific genetic mutations that increase the likelihood of developing the disease. Examples of genetic syndromes linked to leukemia include Down syndrome, Fanconi anemia, and Li-Fraumeni syndrome. Individuals diagnosed with these syndromes should work closely with their healthcare providers to develop a comprehensive monitoring and treatment plan to address their increased risk of leukemia.
Understanding the inherited genetic risk factors associated with leukemia is paramount in identifying individuals who may be at a higher risk. By recognizing the significance of family history and genetic syndromes, healthcare providers can implement appropriate screening and preventive measures to ensure early detection and timely intervention. Stay tuned as we explore further aspects of genetic factors and their impact on the development of leukemia.
The development of leukemia is influenced by various genetic factors, including both inherited and acquired changes. While inherited genetic factors play a significant role in predisposing individuals to this disease, acquired genetic changes can also contribute to the risk of developing leukemia.
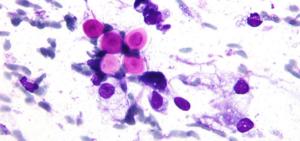
Somatic mutations are genetic alterations that occur after conception and are not inherited from parents. These changes can arise due to various factors such as exposure to radiation, certain chemicals, or even errors during DNA replication. In the context of leukemia, somatic mutations can occur in the cells of the bone marrow, leading to the abnormal proliferation and growth of leukemia cells.
These somatic mutations can affect crucial genes that control cell division, apoptosis (cell death), or DNA repair processes. Such alterations can disrupt the balance between cell growth and cell death, allowing the uncontrolled growth of leukemia cells. Common genes affected by somatic mutations in leukemia include FLT3, NPM1, and TP53. Identification of these somatic mutations can help in diagnosis, prognosis, and selection of targeted therapies for leukemia patients.
Another type of acquired genetic change associated with leukemia is chromosomal abnormalities. These abnormalities involve structural changes or rearrangements of chromosomes, and they can impact the functioning of specific genes or disrupt the overall stability of the genome. Chromosomal abnormalities play a crucial role in the development of various types of leukemia, such as acute lymphoblastic leukemia (ALL) or chronic myeloid leukemia (CML).
The most well-known chromosomal abnormality associated with leukemia is the Philadelphia chromosome, which is commonly found in patients with CML. This chromosomal rearrangement fuses the BCR (breakpoint cluster region) gene on chromosome 22 with the ABL1 (Abelson tyrosine kinase 1) gene on chromosome 9, resulting in the formation of a fusion gene called BCR-ABL1. The BCR-ABL1 fusion gene produces a protein with abnormal kinase activity, driving the uncontrolled growth of leukemia cells.
In addition to the Philadelphia chromosome, there are other chromosomal abnormalities, such as translocations, deletions, and duplications, that are associated with different subtypes of leukemia. These chromosomal changes can have various effects on gene expression and ultimately contribute to the development and progression of leukemia.
Understanding acquired genetic changes and their impact on the risk of developing leukemia is crucial for both research and clinical practice. The identification of specific somatic mutations or chromosomal abnormalities can guide personalized treatment strategies and improve outcomes for leukemia patients.
Credit: www.frontiersin.org
Genetic testing plays a vital role in understanding the risk of developing leukemia and guiding treatment decisions. It involves analyzing a person’s DNA to identify specific genetic changes or mutations that may be associated with the development and prognosis of leukemia. There are two main types of genetic testing in leukemia: diagnostic genetic testing and prognostic genetic testing.
Diagnostic genetic testing is conducted to confirm the presence of leukemia and determine the specific type or subtype of the disease. It helps doctors to make an accurate diagnosis and develop a tailored treatment plan. This type of testing usually involves analyzing bone marrow or blood samples.
During diagnostic genetic testing, various techniques such as fluorescence in situ hybridization (FISH) and polymerase chain reaction (PCR) are used to detect specific genetic changes in leukemia cells. FISH allows researchers to visualize certain genetic alterations, while PCR helps to amplify and analyze specific DNA sequences.
By identifying specific genetic abnormalities, diagnostic genetic testing provides valuable information about the leukemia subtype, which can guide treatment decisions. For example, certain genetic mutations may indicate a higher response to targeted therapies, while others may be associated with a worse prognosis.
Prognostic genetic testing is performed to predict the course of the disease and assess the likelihood of treatment success in individuals with leukemia. It helps doctors to determine the most appropriate treatment approach and optimize patient outcomes.
During prognostic genetic testing, various genetic markers or mutations associated with different prognostic groups are analyzed. These markers provide insight into a patient’s likelihood of achieving remission, risk of disease relapse, and overall survival prospects. The results of prognostic genetic testing help doctors to stratify patients into different risk categories and personalize their treatment plans.
Prognostic genetic testing is particularly important in the management of acute myeloid leukemia (AML), where specific genetic mutations are strongly associated with treatment response. For example, the presence of a mutation in the FLT3 gene may indicate a higher risk of relapse and the need for more aggressive therapies.
Overall, genetic testing in leukemia is a powerful tool that aids in accurate diagnosis and personalized treatment plans. It allows doctors to tailor therapies based on individual genetic profiles, improving the chances of successful treatment outcomes. By understanding the genetic factors contributing to leukemia, healthcare professionals can optimize patient care and provide targeted interventions.
Genetic factors play a crucial role in the development of leukemia, making it essential to understand their implications for treatment and prevention. This comprehensive overview sheds light on the significance of genetic factors in assessing individuals’ risk of developing leukemia, guiding future preventive measures and treatment strategies.
New advancements in the field of precision medicine have revolutionized the treatment of leukemia. By taking into account an individual’s unique genetic factors, healthcare professionals can now tailor treatment plans to specifically target the underlying causes of the disease. This personalized approach not only maximizes the effectiveness of treatment but also minimizes the risk of adverse side effects.
Targeted therapies have emerged as a promising approach in the fight against leukemia. These therapies are designed to specifically attack cancer cells while sparing healthy cells, resulting in fewer side effects. By identifying the genetic mutations driving the development of leukemia cells, targeted therapies can directly target these anomalies. This targeted approach has shown great promise in improving treatment outcomes and extending the lifespan of individuals diagnosed with leukemia.
The goal of precision medicine in leukemia treatment is to identify the specific genetic alterations that contribute to the development and progression of the disease. By doing so, healthcare professionals can choose the most appropriate treatment options, improving the chances of successful outcomes. This individualized approach recognizes that each patient’s leukemia is unique and requires a personalized treatment strategy.
Genetic testing plays a crucial role in identifying individuals who are at a higher risk of developing leukemia. By analyzing an individual’s DNA, healthcare professionals can identify genetic mutations associated with an increased susceptibility to the disease. This information is invaluable in determining preventative measures and designing targeted screening programs to detect leukemia at an early stage.
Identifying high-risk individuals allows for early detection and intervention. Early diagnosis significantly improves treatment outcomes and increases the chances of successful remission. Through routine screening and proactive monitoring, individuals with a higher risk of developing leukemia can receive timely and appropriate interventions, such as targeted therapies or bone marrow transplants, if necessary.
Another crucial aspect of identifying high-risk individuals is providing education and awareness. By informing individuals about their genetic predisposition to leukemia, they can make informed decisions regarding their lifestyle, such as adopting healthy habits and avoiding environmental factors that may further increase their risk. Education empowers individuals to take proactive steps in reducing their chances of developing leukemia and promotes overall well-being.
In conclusion, precision medicine and targeted therapies have opened new avenues in the treatment of leukemia. By considering an individual’s genetic factors, healthcare professionals can design tailored treatment plans for more effective and personalized care. Moreover, identifying high-risk individuals through genetic testing allows for early intervention and education, further improving outcomes and promoting a healthier future.

Credit: www.sciencedirect.com

Credit: www.nejm.org
Genetic risk factors for leukemia involve certain gene mutations, like FLT3, NPM1, and TP53, which increase the likelihood of developing the disease. These mutations affect the normal functioning of cells in the bone marrow, leading to uncontrolled growth of abnormal white blood cells.
The genetic anomaly that increases the risk for developing leukemia is an abnormality in the DNA structure.
The risk of developing leukemia increases due to certain factors such as exposure to high levels of radiation or certain chemicals, having certain genetic disorders or a family history of leukemia.
Leukemia is caused by genetic alterations in bone marrow cells, leading to uncontrolled growth of abnormal white blood cells. These genetic changes can be inherited or acquired during a person’s lifetime.
Overall, it is evident that genetic factors play a significant role in determining the risk of developing leukemia. Understanding these genetic markers and their implications is crucial in identifying individuals at risk and developing targeted prevention strategies. By continuously researching and expanding our knowledge in this field, we can make significant strides in combating this devastating disease and improving the chances of survival for those afflicted.