Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124

Multiple Sclerosis (MS) does not have a set timeline for how long it takes to be fatal. The disease is unpredictable in nature and can progress differently for each individual.
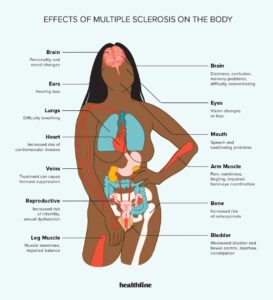
However, MS is not typically considered a direct cause of death. Multiple Sclerosis (MS) is a chronic autoimmune disease affecting the central nervous system. This condition can lead to various physical and cognitive symptoms, such as muscle weakness, fatigue, balance problems, and difficulty with coordination and thinking.
While MS is a lifelong condition, its overall impact and progression can vary significantly from person to person. Some individuals may experience a relatively mild course of the disease, with minimal disability over decades. On the other hand, some may face more severe symptoms that rapidly progress, affecting their quality of life. Despite the potential challenges and complications associated with MS, it is important to note that the disease itself is not typically the direct cause of death. We will explore the factors influencing the timeline of MS and its potential effects on mortality.

Credit: www.healthline.com
Multiple Sclerosis (MS) is a chronic illness affecting the central nervous system that can vary greatly from person to person. The progression and severity of MS is unpredictable and can lead to disability, but the average life expectancy is unaffected and MS itself is not considered fatal.
Multiple Sclerosis (MS) is a chronic and unpredictable autoimmune disease that affects the central nervous system (CNS). In simple terms, it is a disease in which the body’s own immune system attacks the protective covering of nerve fibers (myelin) in the brain and spinal cord. The damaged myelin disrupts the normal flow of electrical impulses between the brain and the rest of the body, leading to a wide range of symptoms.
The exact cause of Multiple Sclerosis is still unknown, but researchers believe that a combination of genetic and environmental factors play a role in its development. Some key factors that may contribute to the onset of MS include:
It is important to note that while these factors may increase the risk of developing MS, they do not guarantee that a person will develop the condition. MS is a complex disease with a variety of contributing factors, and further research is needed to fully understand its causes.
Multiple Sclerosis (MS) is a chronic autoimmune disease that affects the central nervous system. It can cause a wide range of symptoms that vary from person to person. Recognizing these symptoms is crucial for early diagnosis and effective management of the disease. In this section, we will discuss the early symptoms and progressive symptoms of Multiple Sclerosis.
Early symptoms of Multiple Sclerosis are often mild and easily overlooked. Individuals may experience:
As Multiple Sclerosis progresses, the symptoms may become more severe and potentially disabling. Some progressive symptoms include:
It’s important to note that these symptoms can vary in severity and progression from person to person. If you experience any of these symptoms or have concerns about your health, it is crucial to consult a healthcare professional for an accurate diagnosis and appropriate treatment.
In understanding multiple sclerosis (MS), it is essential to grasp the progression types that characterize this chronic neurological condition. MS progression can vary greatly between individuals, with symptoms and severity ranging widely. There are three main types of MS: relapsing-remitting MS, secondary progressive MS, and primary progressive MS. Learning about each type will help shed light on the different ways MS can manifest and progress in the body.
Relapsing-remitting MS (RRMS) is the most common form of multiple sclerosis, accounting for approximately 85% of cases. This type of MS is characterized by periods of relapses, where new symptoms appear or existing ones worsen, followed by periods of remission, where the symptoms partially or completely subside. During remission, the person may experience a partial recovery, resulting in a stable or improved condition.
It is important to note that the duration and frequency of relapses in RRMS can vary significantly among individuals. Some may experience several relapses a year, while others may have longer periods of remission between relapses. The progression of RRMS can be unpredictable, with some individuals remaining in the relapsing-remitting stage for many years, while others may transition to secondary progressive MS.
Secondary progressive MS (SPMS) typically follows relapsing-remitting MS, although it can also occur independently. This stage involves a gradual worsening of symptoms and a decrease in the frequency of relapses. Unlike relapsing-remitting MS, there are typically no distinct periods of remission. Instead, the symptoms become more persistent and slowly progress over time.
In secondary progressive MS, the accumulation of disability becomes more noticeable and may impact daily activities and overall quality of life. However, the rate of progression can vary widely between individuals, with some experiencing a slow and steady decline, and others encountering more rapid deterioration.
Primary progressive MS (PPMS) accounts for around 10-15% of all MS cases and is characterized by a gradual and steady progression of symptoms from the onset. Unlike relapsing-remitting or secondary progressive MS, there are no distinct periods of remission in primary progressive MS. Individuals with PPMS may experience subtle changes in their symptoms, which worsen over time, resulting in a gradual loss of physical and cognitive function.
It is important to note that the rate of progression in primary progressive MS can vary greatly among individuals. Some may experience a relatively slow decline, while others may encounter a more rapid deterioration. PPMS tends to affect individuals at an older age compared to relapsing-remitting and secondary progressive MS.
The progression of multiple sclerosis can vary significantly from person to person. While some individuals may experience periods of relapses and remission, others may face a gradual and steady progression of symptoms. Understanding the different types of MS and their respective progression patterns can provide valuable insights into the disease’s course, helping individuals and healthcare professionals manage their condition more effectively.

Credit: www.healthline.com
Multiple Sclerosis (MS) does not have a predictable timeline for causing death. The long-term outlook varies from person to person, with factors such as disease progression, treatment effectiveness, and overall health influencing outcomes. Regular medical monitoring, early intervention, and a healthy lifestyle can potentially enhance quality of life and lengthen survival for MS patients.
Living with multiple sclerosis (MS) can present long-term challenges, impacting the life expectancy and quality of life of those affected. Understanding the long-term outlook for MS patients is crucial in providing support and insight into the potential impact of the condition.
Despite the challenges posed by MS, individuals diagnosed with the condition have a life expectancy that approaches that of the general population. The median life expectancy for someone with MS is around 7 years lower than the overall population. Additionally, advancements in treatments and healthcare have improved outcomes, with many patients living full, satisfying lives for decades after diagnosis.
The quality of life for MS patients can vary widely depending on the progression and severity of the condition. Some individuals experience minimal impact on their daily activities, while others may require significant assistance with mobility, communication, and self-care. Lifestyle adjustments and access to appropriate healthcare and support services can significantly impact the quality of life for those living with MS.
With a focus on holistic care, including medical interventions, lifestyle modifications, and emotional support, individuals can optimize their quality of life and maintain a sense of independence and fulfillment.
In conclusion, it’s crucial to acknowledge the unique experiences of each individual with MS and prioritize comprehensive care and support to enhance their long-term outlook and overall well-being.
Multiple sclerosis (MS) is a chronic disease that varies in progression and impact. It is not typically fatal, but certain factors such as age, gender, and disease subtype can influence the rate and severity of MS progression. Early diagnosis and proper treatment can help manage symptoms and slow disease progression.
Factors affecting the progression of multiple sclerosis (MS) are varied and can impact the course of the disease. Age, gender, genetics, and environmental factors all play a role in determining how MS may progress in an individual. Understanding these factors can provide valuable insight into the severity and speed of disease progression as well as aid in the development of personalized treatment plans.
Age plays a pivotal role in the progression of MS. Younger individuals at the time of diagnosis often experience a milder disease course, with longer intervals between relapses. Conversely, older patients may face a more rapid progression of disability. The impact of age underscores the importance of early diagnosis and intervention, particularly in younger patients.
Gender has been identified as a factor influencing the progression of MS. Women are more likely to develop the condition than men, and they may experience more frequent relapses and a higher likelihood of progressing to the secondary progressive stage. This disparity in gender highlights the need for targeted research and interventions to address the unique challenges faced by female patients.
The role of genetics in MS progression is complex and multifaceted. Genetic predisposition is known to contribute to the risk of developing MS, and certain genetic variations have been linked to a more aggressive disease course. Understanding the genetic underpinnings of MS can offer valuable insights into individual prognosis and inform personalized treatment strategies.
Environmental factors, such as exposure to certain viruses, smoking, and vitamin D levels, have been implicated in influencing the progression of MS. These factors can interact with genetic predisposition to modulate the course of the disease. Identifying and addressing environmental influences is crucial in managing MS and mitigating its impact on patients.

Credit: www.amazon.com
It’s difficult to pinpoint an exact timeframe for Multiple Sclerosis (MS) to disable someone as it varies from person to person. The progression of MS differs, and some people may experience mild symptoms for many years while others may become disabled more rapidly.
Early diagnosis and treatment can help manage the condition and slow down disability progression.
The speed at which multiple sclerosis (MS) worsens varies for each person. It can progress slowly over many years or rapidly within a short time. The progression of MS depends on individual factors and the type of MS a person has.
Regular consultation with a healthcare professional can help in monitoring its progression.
The life expectancy of MS patients varies, but on average it’s around 7 to 10 years shorter compared to the general population. Early diagnosis and proper treatment may help extend life expectancy. Regular medical care and a healthy lifestyle are essential for managing the disease effectively.
Yes, multiple sclerosis (MS) can pose a risk to life. MS is a chronic neurological disease that affects the central nervous system, and the severity of symptoms can vary. While MS itself is not usually fatal, complications and secondary conditions can contribute to mortality in rare cases.
The duration of multiple sclerosis (MS) and the impact it has on one’s life can vary greatly from person to person. While it is a chronic and progressive disease, it does not necessarily lead to death. With advancements in treatment and management strategies, individuals with MS can lead fulfilling lives and maintain their overall well-being.
Remember to consult with your healthcare professional for personalized guidance on living with MS.