Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
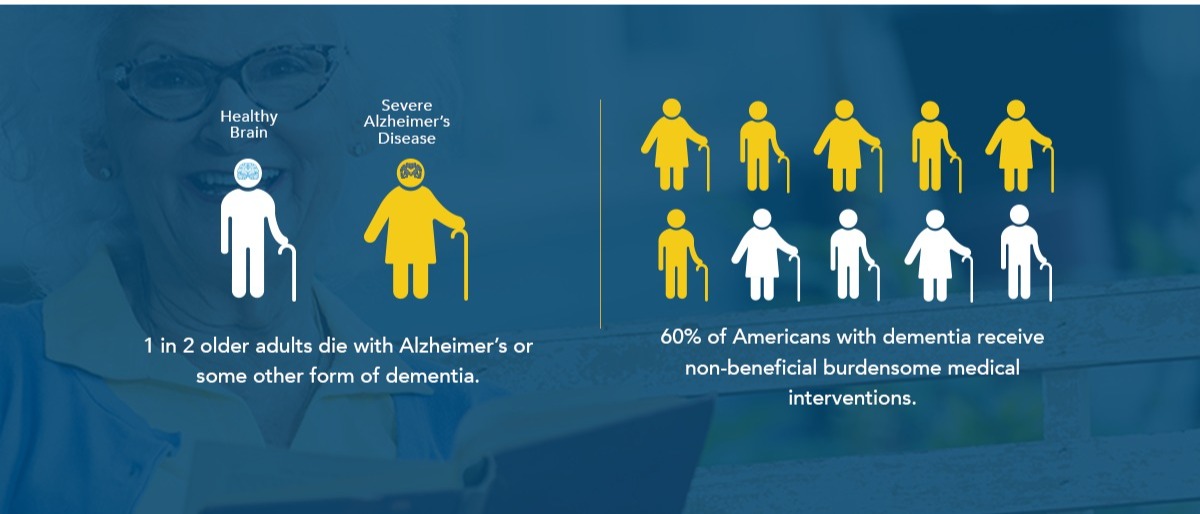
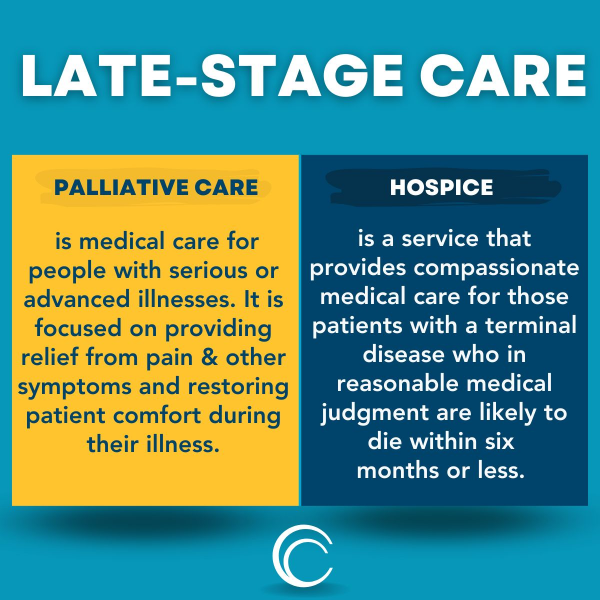
Palliative care for advanced dementia focuses on comfort and quality of life. It manages pain and symptoms without aiming for a cure.
Palliative care plays a crucial role in providing support for individuals with advanced dementia. It offers relief from the distressing symptoms and stress associated with the illness. This holistic approach prioritizes the patient’s and their family’s needs and preferences, emphasizing emotional, social, and spiritual well-being.
By addressing the complex challenges faced by those with advanced dementia, palliative care ensures dignity and compassion are at the forefront of treatment, even as curative options are no longer pursued. The goal is to improve life quality for both the patient and their caregivers, making each day as fulfilling as possible within the context of the disease.
Credit: www.compassionandchoices.org
Welcome to our deep dive into ‘Introduction to Palliative Care in Advanced Dementia’. In this journey, we unravel the complexities surrounding advanced dementia. We spotlight the compassionate approach of palliative care. Here, we outline how it aims to enhance life quality for those embarking on the later stages of this condition.
Dementia describes a group of symptoms affecting memory, thinking, and social skills. It progresses over time. Early stages may involve forgetfulness. Advanced stages can lead to complete dependency.
The goals of palliative care in dementia are pivotal. Care aims to:
These principles guide the path to ensuring a dignified, respectful journey for every patient.
Challenges in Providing Palliative Care to Dementia Patients
As dementia progresses to its advanced stages, palliative care becomes essential. This specialized medical care focuses on providing relief from the symptoms and stress of a serious illness. Dementia poses unique challenges due to the nature of the disease, which deeply affects cognitive functions. Ensuring dignity and comfort to patients with advanced dementia requires careful consideration of several sensitive issues.
One of the biggest challenges in palliative care for dementia patients is the decline in communication abilities. This decline can hinder the patient’s capacity to express their needs and participate in their care decisions. Understanding non-verbal cues becomes crucial for caregivers and medical professionals to provide appropriate care.
End-of-life decisions often come with heavy ethical implications. Decisions about the use of feeding tubes, resuscitation, and hospitalization can be deeply complex. It’s critical to balance the patient’s best interests with respect for their autonomy, even when they cannot make their wishes known directly.
Family members play a pivotal role in decision-making for dementia patients. The dynamic of each family can greatly affect the care process, with different views and emotions coming into play. Open communication and support are key to navigate these delicate situations and provide the best care possible.
Recognizing pain and discomfort in patients who cannot speak is a significant challenge. Caregivers must use observation skills and alternative strategies to assess signs of distress. Tools such as pain scales adapted for non-verbal patients can be instrumental in ensuring the patient remains as comfortable as possible.
Dealing with advanced dementia requires a tailored approach to care.
Comprehensive Care Approaches address each patient’s needs.
Every individual with dementia is unique.
Personalized care plans ensure their specific needs are met.
Non-pharmacological interventions focus on comfort without medication.
These may include:
When symptoms are severe, pharmacological management might be needed.
Medications can help:
Support services are vital for both patients and families.
Available services could include:
Palliative care for advanced dementia demands an extraordinary level of teamwork and understanding.
A collaborative and multidisciplinary approach ensures that care is comprehensive and fully attuned to the patient’s needs.
Every team member plays a critical role, addressing not just physical symptoms but also the emotional and spiritual well-being of patients and their families.
A palliative care team brings together diverse professionals, each with a unique skill set.
Combining medical treatment with emotional support creates a holistic care plan.
This approach respects the person beyond their illness.
Providing families and caregivers with proper training is crucial.
Workshops and educational materials build their skills and confidence.
When a loved one faces advanced dementia, care decisions get complicated. Ethical and legal considerations take center stage, ensuring dignity and respect stay intact. This delicate time requires understanding laws and applying ethical principles to care.
Advance directives guide care when a person can’t express their wishes. Living wills outline what medical treatment someone wants or doesn’t want. In dementia, it’s crucial to establish these documents early. They safeguard personal choices and provide clear instructions to caregivers and medical staff.
A DNR order tells health professionals not to perform CPR if a patient stops breathing or their heart stops. It’s a personal decision, one that should be respected by all care providers. Families must discuss DNR orders openly. This ensures everyone understands and honors the patient’s wishes.
| Topic | Details |
|---|---|
| What it Includes | No CPR or advanced life support interventions |
| How to Set Up | In consultation with healthcare providers |
Patients with dementia retain their legal rights. They deserve to receive care consistent with their values. Caregivers also have rights. They must have the resources and support needed to fulfill their role. Understanding these legal rights helps avoid conflict and ensures compassionate care.
Palliative care often changes lives, especially for those with advanced dementia. This post shines a light on real-world examples where this specialized care has made a difference. Read these case studies and personal stories to understand its profound impact.
Meet John: At 82, dementia dimmed his vibrant life. With palliative care, John’s days became filled with music, his favorite. Nurses knew his playlist by heart. Pain management improved his comfort. John smiled more, showing the care’s true value.
Linda’s story: Her mother’s dementia journey was tough. Palliative care brought relief. Daily stress reduced. Linda found support in managing her mother’s needs. Together, they navigated the dementia pathway with dignity and love.
In New England, a hospice introduced an innovative program. It blended art therapy with palliative care. Dementia patients engaged in painting. It improved communication and sparked joy in their eyes. This program set a benchmark for creativity in care.
Challenges and opportunities define the evolving landscape of palliative care for advanced dementia. Families and caregivers often navigate a complex path, balancing quality of life with medical care. As we look to the future, addressing these challenges presents clear opportunities to enhance care quality and accessibility for one of our most vulnerable populations.
Universal access to palliative care remains the cornerstone for improving the lives of dementia patients. Currently, disparities in care quality and availability pose significant obstacles. Expanding palliative services across communities can bridge this crucial gap.
Pivotal research is the key to unlocking innovative care strategies for dementia.
Healthcare policy adaptations must underscore dementia care advancement. With strategic reforms, systems can better support the unique needs of dementia care.
| Policy Target | Expected Outcome |
|---|---|
| Better funding models | Enhanced care delivery |
| Regulatory support for caregivers | Increased caregiver resources |
Yes, individuals with dementia may qualify for palliative care to manage symptoms and improve quality of life.
Stage 7 dementia, the final phase, is marked by severe cognitive decline. Individuals lose the ability to communicate, recognize loved ones, and require help with all daily activities, including walking and eating.
The life expectancy for someone with advanced dementia typically ranges from 1 to 5 years. Factors such as age and overall health can influence this duration.
Individuals with dementia can receive palliative care from diagnosis until end of life, which may span months to several years. The duration is tailored to each person’s unique needs and disease progression.
Understanding palliative care is crucial for those facing advanced dementia. This compassionate approach prioritizes comfort, dignity, and quality of life. Families and caregivers can find solace and support, ensuring their loved ones receive the best care possible. Remember, palliative care is about living as fully as possible, despite serious illness.
Embracing this journey together can be profoundly rewarding.

