Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
Coronary Artery Disease involves blockages in arteries, causing restricted blood flow, while Coronary Artery Calcification is the build-up of calcium deposits in the arteries. These conditions can increase the risk of heart attacks and other cardiovascular issues.
Coronary Artery Disease is predominantly characterized by the narrowing of the coronary arteries due to plaque build-up, which restricts blood flow to the heart muscle. On the other hand, Coronary Artery Calcification refers to the presence of calcium deposits within the arterial walls, indicating atherosclerosis development and potential risks of coronary events.
Understanding the distinctions between these conditions is crucial for effective prevention and management of cardiovascular health. By recognizing the unique features of each condition, individuals can take proactive steps to minimize their risk factors and maintain a healthy heart.
Credit: www.nature.com
Coronary Artery Disease is a condition caused by narrowing of the blood vessels leading to the heart. On the other hand, Coronary Artery Calcification is the buildup of calcium in the coronary arteries, indicating the presence of atherosclerosis.
Definition
Coronary Artery Disease (CAD) occurs when the blood vessels that supply the heart with oxygen-rich blood become narrowed or blocked due to plaque buildup. This restricts blood flow to the heart.
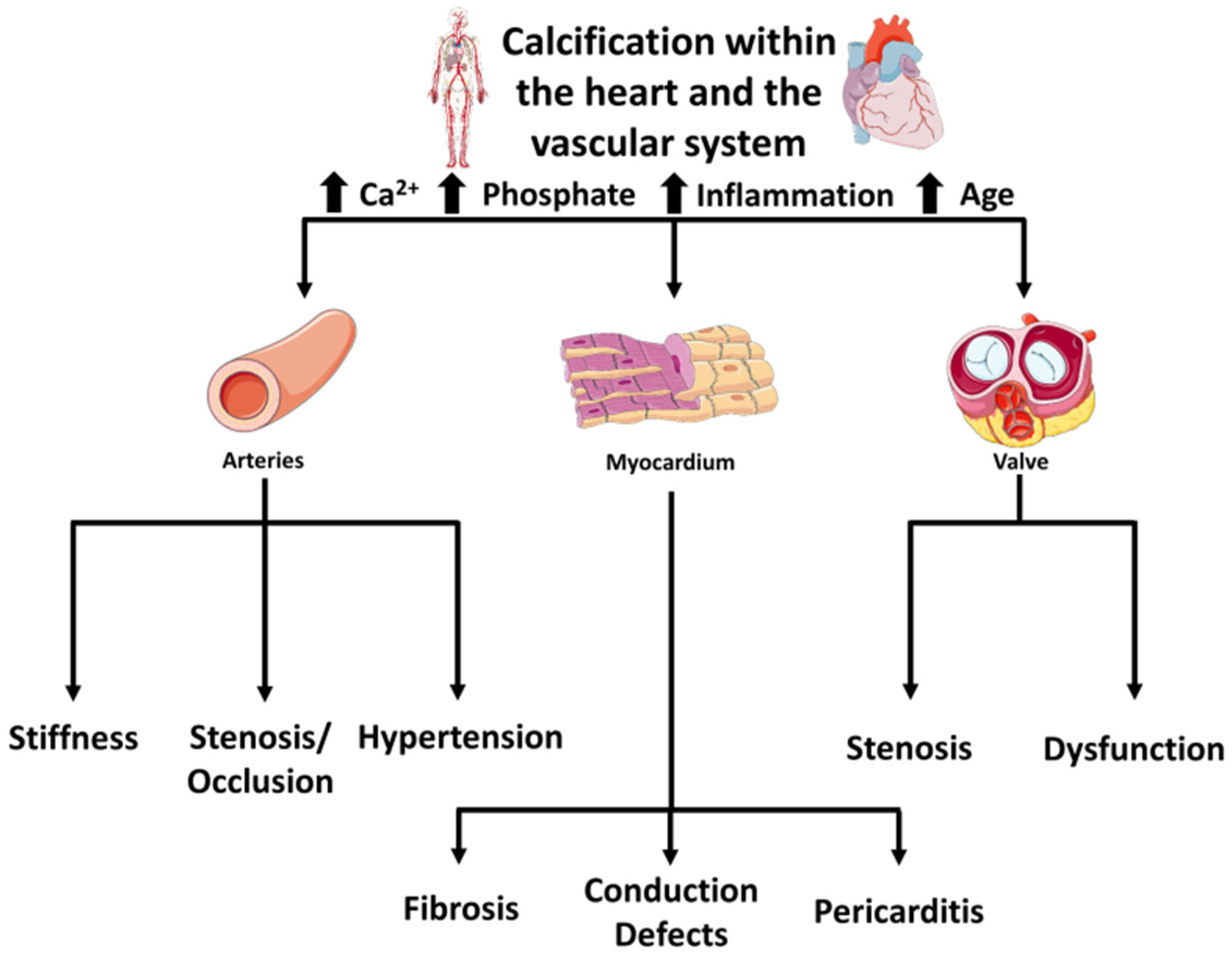
Coronary artery calcification occurs when there is a build-up of calcium in the walls of the coronary arteries. This calcification is often associated with the development of coronary artery disease (CAD), a common heart condition that can lead to serious complications.
Coronary artery calcification is the accumulation of calcium in the walls of the coronary arteries, which supply blood to the heart muscle.
Coronary Artery Disease is a condition marked by plaque buildup in the arteries, leading to reduced blood flow. On the other hand, Coronary Artery Calcification refers specifically to the accumulation of calcium deposits in the arteries, which can be a precursor to coronary artery disease.
Coronary artery disease (CAD) and coronary artery calcification (CAC) are two cardiovascular conditions that can affect the heart’s blood vessels. While they may sound similar, there are significant differences between the two conditions in terms of their location and nature, underlying mechanisms, progression, and diagnosis.
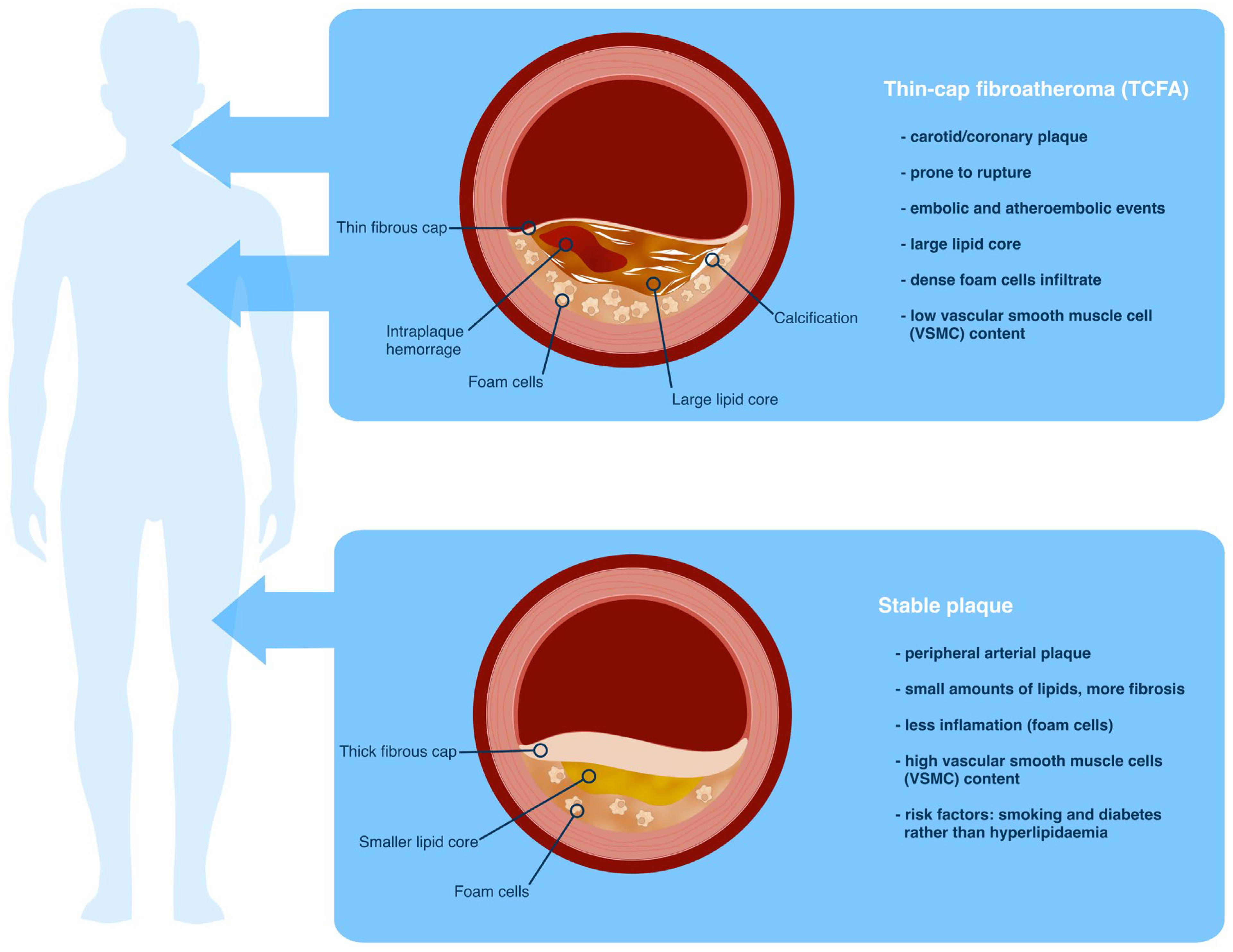
The main difference between CAD and CAC lies in their location and nature. Coronary artery disease refers to the narrowing or blockage of the coronary arteries, which supply oxygen-rich blood to the heart muscle. This narrowing can be caused by the buildup of plaque, comprised of fat, cholesterol, and other substances, along the artery walls.
In contrast, coronary artery calcification primarily involves the buildup of calcium deposits within the walls of the coronary arteries. These deposits can harden over time and contribute to the narrowing of the arteries, reducing blood flow to the heart.
The underlying mechanisms for CAD and CAC also differ. CAD often develops as a result of atherosclerosis, a condition characterized by the accumulation of fatty deposits within the artery walls. These deposits can lead to the formation of plaques, which can rupture and trigger blood clot formation, potentially causing a heart attack.
Coronary artery calcification, on the other hand, occurs due to the buildup of calcium within the arterial walls. The exact mechanisms behind this process are still not fully understood, but it is believed to involve a combination of inflammation and the body’s attempt to repair damaged vessels.
The progression of CAD and CAC also differs. In coronary artery disease, the narrowing or blockage of the coronary arteries can occur gradually over time, leading to symptoms such as chest pain (angina) or shortness of breath. If left untreated, CAD can progress to a complete blockage of the arteries, resulting in a heart attack.
On the other hand, coronary artery calcification tends to progress at a slower rate and may not cause symptoms until the arteries are significantly narrowed. It is also worth noting that individuals with CAC may not always develop CAD, as the presence of calcification does not necessarily indicate the presence of plaque buildup.
Diagnosing CAD and CAC involves different methods. CAD is typically diagnosed through a combination of medical history evaluation, physical examination, and diagnostic tests such as an electrocardiogram (ECG), stress test, or coronary angiography. These tests help identify the presence and severity of arterial blockages.
On the other hand, coronary artery calcification is commonly assessed using a coronary calcium score, derived from a specialized computed tomography (CT) scan. This score provides an estimate of the amount of calcification in the coronary arteries and helps determine an individual’s risk for future cardiovascular events.
While both CAD and CAC involve the heart’s blood vessels, their differences in location and nature, underlying mechanisms, progression, and diagnosis highlight the need for precise evaluation and treatment strategies for these distinct conditions.
Understanding the difference between coronary artery disease (CAD) and coronary artery calcification (CAC) is crucial for effectively managing heart health. Both conditions have distinct risk factors and prevention strategies that can help individuals minimize their risk of developing these potentially serious cardiovascular diseases. By recognizing the unique characteristics of each condition, individuals can take proactive steps to protect their heart health and reduce the likelihood of experiencing related complications.
CAD is primarily influenced by lifestyle factors such as smoking, high cholesterol levels, high blood pressure and diabetes. In contrast, CAC is the accumulation of calcium within the coronary arteries, often associated with aging, male gender, and family history of CAC. Individuals with a history of obesity and sedentary lifestyle may also face an increased risk of developing CAC.
For CAD, lifestyle modifications such as regular exercise, healthy diet, and stress management can significantly reduce the risk of development. Additionally, quitting smoking, monitoring cholesterol levels, and managing blood pressure and diabetes are critical preventive measures. To prevent CAC, it’s important to focus on overall cardiovascular health through habits like regular physical activity, a balanced diet, and regular health check-ups to assess risk factors and address any potential concerns.
Treatment of coronary artery disease (CAD) and coronary artery calcification (CAC) involves a variety of options ranging from lifestyle changes to surgical interventions. Understanding the differences in their treatment approaches is crucial for effectively managing these conditions.
Adopting a heart-healthy diet and engaging in regular physical activity are pivotal in managing both CAD and CAC. Reducing sodium intake, limiting saturated fat and cholesterol, and consuming more fruits and vegetables can help support heart health. Regular exercise promotes cardiovascular fitness and weight management, aiding in the prevention and control of these conditions.
Medications play a significant role in managing CAD and CAC. Cholesterol-lowering drugs such as statins are commonly prescribed to lower LDL cholesterol. Aspirin is often recommended for antiplatelet effects to reduce the risk of blood clots. Additionally, other medications like beta-blockers and ACE inhibitors may be prescribed to manage symptoms and improve heart function.
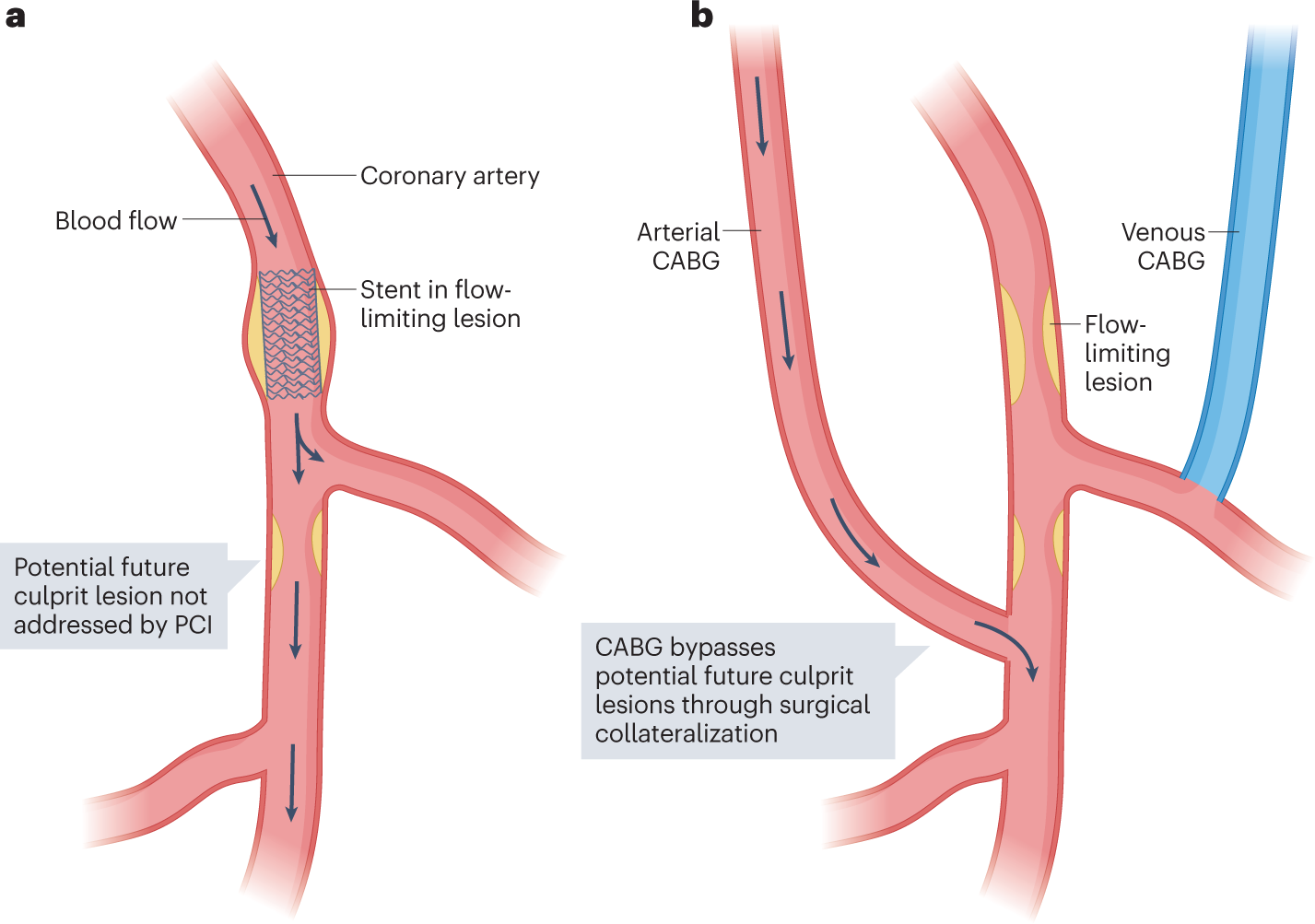
In cases of CAD and CAC, surgical interventions may be necessary. Procedures such as angioplasty with stent placement can help open blocked or narrowed arteries. Coronary artery bypass grafting (CABG) may be recommended for more severe cases, providing a new pathway for blood to flow to the heart muscle.
Credit: www.mdpi.com
Both coronary artery disease (CAD) and coronary artery calcification (CAC) can have serious complications that can impact a person’s health and quality of life. It is essential to understand the potential complications associated with these conditions in order to take appropriate measures for prevention and management.
Coronary artery disease, also known as atherosclerosis, occurs when the arteries that supply blood to the heart become narrowed or blocked due to the buildup of plaque. This can lead to several complications, including:
Coronary artery calcification refers to the buildup of calcium deposits within the walls of the coronary arteries. While it is one of the markers for the presence of CAD, it can also have its own set of complications. Some of the potential complications of coronary artery calcification include:
It is important to note that both coronary artery disease and coronary artery calcification share some common complications, such as an increased risk of heart attack and other cardiovascular events. However, understanding the specific complications associated with each condition can help healthcare providers tailor prevention and treatment strategies based on individual patient needs.

Credit: citoday.com
Coronary artery disease can cause chest pain, shortness of breath, and fatigue. It may also manifest as nausea, dizziness, and heart palpitations. Seeking medical advice for proper diagnosis and treatment is crucial for managing the symptoms effectively.
Coronary artery calcification is commonly diagnosed through a non-invasive imaging test called a coronary artery calcium scan. This scan uses a special X-ray machine to detect and measure calcium-containing plaque in the arteries, indicating the presence of coronary artery calcification.
Yes, lifestyle modifications like regular exercise, maintaining a healthy diet, quitting smoking, and managing stress can significantly reduce the risk of developing coronary artery disease. These changes can also help manage other risk factors such as high cholesterol and blood pressure, promoting overall heart health.
To summarize, although coronary artery disease and coronary artery calcification may appear similar, they have distinct differences. Coronary artery disease involves the narrowing and blockage of the heart’s arteries due to a buildup of plaque, while coronary artery calcification refers to the deposition of calcium within the artery walls.
Understanding these disparities is crucial for accurate diagnosis and effective treatment. By staying informed and taking preventative measures, individuals can minimize their risk of developing these conditions and maintain a healthy heart.

