Physical Address
304 North Cardinal St.
Dorchester Center, MA 02124
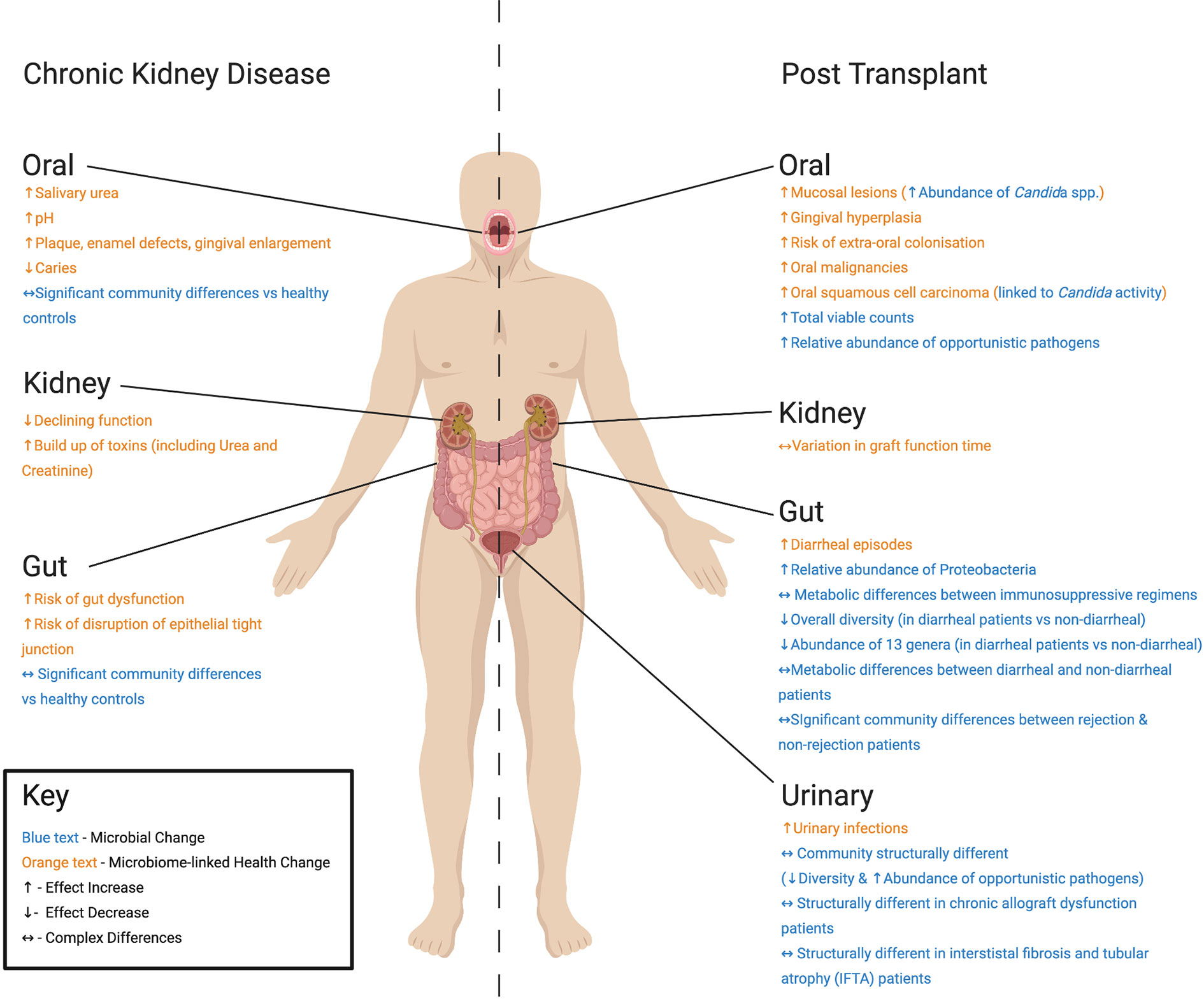
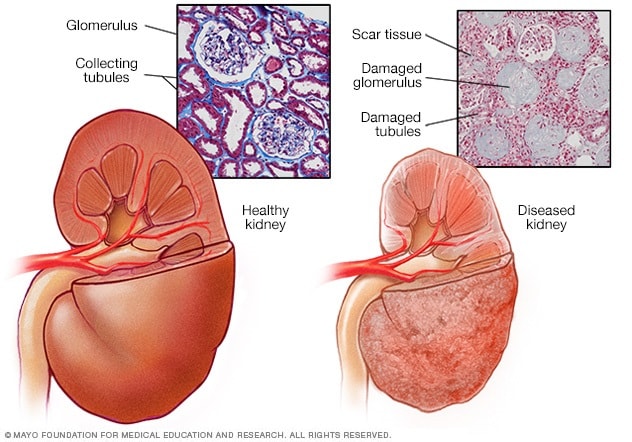
Kidney disease is a general term that includes any condition affecting the kidneys, while chronic kidney disease specifically refers to a long-term, progressive condition that impairs kidney function. It is crucial to understand the difference between these two terms to accurately diagnose and treat the specific kidney condition.
Kidney disease encompasses a range of conditions that affect the kidneys’ function, including infections, cysts, kidney stones, and tumors. On the other hand, chronic kidney disease is characterized by the gradual loss of kidney function over time, often leading to permanent kidney failure.
Understanding the precise nature of the kidney problem is essential for effective management and prevention of further complications. We will explore the disparities between kidney disease and chronic kidney disease, their symptoms, causes, risk factors, and potential treatment options to provide a comprehensive overview for better understanding and management of these conditions.
Kidney disease and chronic kidney disease are often used interchangeably, but they are distinct health conditions with different signs and symptoms. Understanding the differences is crucial for early detection and management. Here’s a breakdown of the signs and symptoms to help distinguish between the two:
Kidney disease, also known as acute kidney injury, can manifest with various signs, including:
Chronic kidney disease (CKD) often progresses slowly over time and may exhibit the following symptoms:

Credit: www.health.harvard.edu
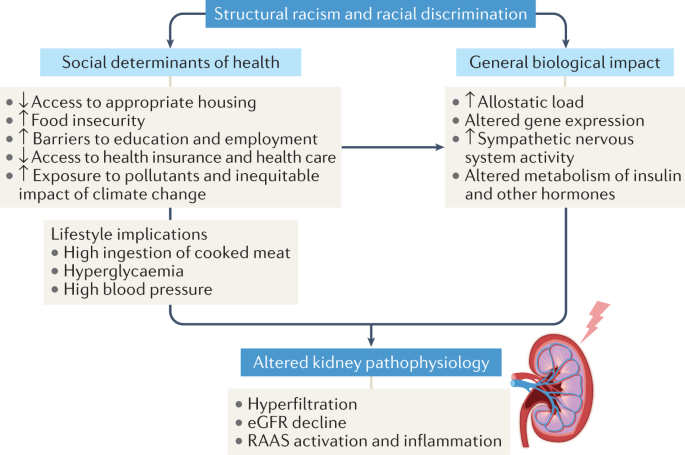
Kidney disease and chronic kidney disease are often used interchangeably, but they are actually two distinct conditions. Understanding the differences between them can help individuals recognize and seek appropriate medical care for their specific condition. One important aspect of these conditions is their causes. Here, we will examine the factors contributing to kidney disease and the causes of chronic kidney disease.
Kidney disease can be caused by a variety of factors. Some of the most common reasons include:
Chronic kidney disease, on the other hand, is characterized by the gradual loss of kidney function over time. The main causes of chronic kidney disease are:
In the process of diagnosing kidney diseases, medical professionals use specific tests and diagnostic procedures to determine the nature and severity of the condition. Understanding the difference in how kidney disease and chronic kidney disease are diagnosed is essential for effective management and treatment.
Kidney disease is typically diagnosed through a series of tests that evaluate the functionality and health of the kidneys. These tests may include:
The diagnostic process for chronic kidney disease involves a more comprehensive approach due to the long-term nature of the condition. It includes:
Credit: www.nature.com
Chronic kidney disease refers to the gradual loss of kidney function over time, leading to permanent kidney damage. It can result from various health conditions and significantly increases the risk of kidney failure. In contrast, kidney disease encompasses a broader range of conditions that impact the kidneys, including acute and chronic issues.
Managing kidney disease involves several approaches that aim to slow down its progression and alleviate symptoms. A combination of lifestyle modifications, medication, and regular follow-ups with healthcare professionals is crucial. Here are some key approaches for kidney disease management:
1. Healthy lifestyle: Maintaining a healthy lifestyle plays a pivotal role in managing kidney diseases. Adopting a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help regulate blood pressure and blood sugar levels, reducing the burden on the kidneys. Staying hydrated by drinking an adequate amount of water throughout the day is also essential.
2. Regular exercise: Engaging in regular physical activity not only helps maintain overall health but also promotes proper kidney function. Exercising for at least 30 minutes a day can help control weight, prevent high blood pressure, and improve blood circulation.
3. Medication: Depending on the type and stage of kidney disease, medication may be prescribed to manage symptoms and slow down the progression of the condition. These medications may include angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), diuretics, and phosphate binders.
4. Strict blood pressure control: Kidney disease often goes hand in hand with high blood pressure. Therefore, maintaining blood pressure within a healthy range is crucial. Healthcare professionals may prescribe antihypertensive medications and recommend lifestyle modifications to control blood pressure effectively.
5. Diabetes management: For individuals with diabetes-related kidney disease, proper management of blood sugar levels is essential. Consistently monitoring blood glucose levels, following a diabetic diet, taking prescribed medications, and exercising regularly can help prevent further kidney damage.
Chronic kidney disease (CKD) requires specific therapies tailored to individual needs. The primary goal of these therapies is to slow down CKD’s progression, manage complications, and address underlying causes. Here are some common therapies used for managing chronic kidney disease:
1. Dialysis: Dialysis is a treatment that helps remove waste products and excess fluid from the bloodstream when the kidneys are no longer able to function adequately. There are two main types of dialysis: hemodialysis and peritoneal dialysis. Hemodialysis involves filtering the blood through a machine, while peritoneal dialysis uses the lining of the abdomen to filter waste.
2. Kidney transplant: For individuals with end-stage renal disease (ESRD), a kidney transplant may be the most suitable treatment option. This procedure involves surgically replacing a non-functioning kidney with a healthy kidney from a living or deceased donor. Kidney transplants offer the opportunity for a better quality of life and decreased dependence on dialysis.
3. Nutritional therapy: A registered dietitian can create a personalized nutritional plan for individuals with chronic kidney disease. This therapy focuses on managing protein, sodium, potassium, and phosphorus intake to maintain optimal kidney function and prevent complications.
4. Anemia management: Chronic kidney disease often leads to anemia, a condition characterized by a shortage of red blood cells. Healthcare professionals may prescribe medications or recommend iron supplements to manage anemia and promote healthy blood cell production.
Remember, these approaches and therapies should be discussed with a healthcare professional to determine the most appropriate treatment plan personalized for your specific condition. Regular monitoring and follow-ups are essential to ensure the management of kidney disease or chronic kidney disease remains effective over time.
Kidney disease and chronic kidney disease are two distinct conditions. The former refers to any abnormality in kidney function, while the latter specifically involves long-term damage. Preventive measures such as maintaining a healthy diet, staying hydrated, and regular exercise can help reduce the risk of developing these conditions.
Kidney disease is a serious health condition that can lead to kidney failure if left untreated. However, there are several preventive measures you can take to reduce the risk of developing kidney disease. By adopting a healthy lifestyle and making smart choices, you can protect your kidneys and maintain their optimal function. Here are some key preventive measures to consider:
Chronic kidney disease (CKD) refers to the gradual and irreversible deterioration of kidney function over time. While some factors that contribute to kidney disease are beyond our control, there are proactive strategies you can adopt to prevent chronic kidney disease and preserve your kidney health:

Credit: www.medicalnewstoday.com
The distinction between Kidney Disease and Chronic Kidney Disease lies in the duration and severity of the condition. Kidney Disease can be acute, sudden, and potentially reversible, while Chronic Kidney Disease is long-term, progressive, and often irreversible, requiring ongoing management to maintain kidney function.
Understanding this difference is crucial for proper diagnosis and treatment planning.
Kidney disease can lead to various complications that impact overall health. Complications may include high blood pressure and fluid retention.
Complications can also result in electrolyte imbalances and anemia, affecting energy levels. Bone diseases can develop due to impaired kidney function.
Chronic Kidney Disease brings about specific complications such as cardiovascular issues and weakened immune system.
Complications may involve elevated potassium levels and acidosis, affecting multiple body systems. Anemia and bone disorders are common in chronic cases.
Complications in Chronic Kidney Disease require careful monitoring and management.
The symptoms of kidney disease may include fatigue, changes in urine output, swelling in the legs and ankles, persistent itching, and high blood pressure.
While there is no cure for kidney disease, it can be managed and slowed down through medication, lifestyle changes, and dialysis or kidney transplant in cases of end-stage kidney disease.
Kidney disease can be caused by various factors including diabetes, high blood pressure, kidney infections, certain medications, autoimmune diseases, and inherited conditions.
Chronic kidney disease is usually diagnosed through blood tests that measure kidney function, urine tests to check for protein or blood in the urine, and imaging tests like ultrasound or CT scan.
Kidney disease and chronic kidney disease differ in severity and progression, affecting kidney function. Understanding these distinctions will promote early detection and appropriate management. Maintaining a healthy lifestyle and regular check-ups can mitigate the risks associated with these conditions. Stay informed and proactive about kidney health.